
Demam denggi adalah sejenis penyakit jangkitan virus yang merebak melalui gigitan nyamuk Aedes aegypti yang telah dijangkiti.
Terdapat empat (4) jenis virus yang boleh menyebabkan demam denggi (DEN 1, DEN 2, DEN 3 dan DEN 4).
Jangkitan oleh salah satu jenis virus akan memberikan imuniti terhadap virus jenis itu sahaja, jika individu tinggal di kawasan jangkitan denggi, mereka boleh di jangkiti lebih dari sekali seumur hidupnya.
Bagaimanakah untuk mengetahui saya berkemungkinan menghidap demam denggi?
Pesakit akan mengalami tanda-tanda dan gejala selepas 5-6 hari gigitan nyamuk seperti:
- Demam panas
- Sakit kepala
- Sakit tulang belakang
- Sakit sendi-sendi
- Loya dan muntah-muntah
- Sakit biji mata
- Ruam
Apakah yang akan terjadi sekiranya saya tidak mendapatkan rawatan?
Demam denggi terdiri daripada demam denggi biasa atau demam denggi berdarah yang boleh membawa maut.
Demam denggi berdarah mempunyai tanda-tanda di atas dan juga pendarahan seperti:
- Mudah lebam
- Pendarahan di bawah kulit, pada hidung atau gusi
- Ia boleh diikuti dengan pendarahan seluruh badan yang juga membawa maut
Apakah rawatan untuk demam denggi?
Masih tiada rawatan khas untuk demam denggi. Pesakit yang mengalami tanda-tanda dan menunjukkan gejala-gejala demam denggi hendaklah mendapatkan rawatan segera. Pesakit akan diberikan ubat demam dan dinasihatkan berehat serta digalakkan minum air. Pesakit akan dimasukkan ke dalam wad sekiranya disyaki menghidap demam denggi berdarah.
Apakah perlu saya lakukan untuk mencegah demam denggi?
Terdapat pelbagai jenis cara untuk mencegah demam denggi :
- Memastikan tiada tempat pembiakan nyamuk
- Membuang bekas yang boleh menakung air
- Pastikan tangki air, bekas tadahan hujan seharusnya ditutup
- Pastikan pasu-pasu bunga dan bekas tadahan dibuang airnya sekurang-kurangnya seminggu sekali
- Pastikan saliran atap sentiasa mengalir
- Membela ikan di dalam kolam ikan untuk mengurangkan jentik-jentik
- Menggunakan semburan serangga untuk membunuh nyamuk
- Mengambil langkah-langkah melindungi diri untuk mengelakkan gigitan nyamuk seperti
- Pastikan tingkap dan pintu sentiasa ditutup
- Sapukan ubat penghalau nyamuk pada anggota terdedah kepada gigitan nyamuk
- Memakai baju berwarna cerah dan berlengan panjang dan seluar panjang sewaktu keluar rumah
- Pasangkan ubat lingkaran nyamuk dan ubat nyamuk elektrik di kawasan tertutup

When your parents were young, people could buy cigarettes and smoke pretty much anywhere — even in hospitals! Ads for cigarettes were all over the place. Today we’re more aware about how bad smoking is for our health. Smoking is restricted or banned in almost all public places and cigarette companies are no longer allowed to advertise on TV, radio, and in many magazines.
Almost everyone knows that smoking causes cancer, emphysema, and heart disease; that it can shorten your life by 10 years or more; and that the habit can cost a smoker thousands of dollars a year. So how come people are still lighting up? The answer, in a word, is addiction.
Once You Start, It’s Hard to Stop
Smoking is a hard habit to break because tobacco contains nicotine, which is highly addictive. Like heroin or other addictive drugs, the body and mind quickly become so used to the nicotine in cigarettes that a person needs to have it just to feel normal.
People start smoking for a variety of different reasons. Some think it looks cool. Others start because their family members or friends smoke. Statistics show that about 9 out of 10 tobacco users start before they’re 18 years old. Most adults who started smoking in their teens never expected to become addicted. That’s why people say it’s just so much easier to not start smoking at all.
Hookahs and E-Cigarettes
It’s not only cigarettes that get people dependent on tobacco. Hookahs, staples of Middle Eastern café society, are water pipes used to smoke tobacco through a hose with a tapered mouthpiece. There’s a myth going around that hookahs are safer because the smoke is cooled when it passes through the water.
But take a look at the black, resinous gunk that builds up in a hookah hose. Some of that gets into users’ mouths and lungs. Indeed, experts say hookahs are no safer than cigarettes — and since they don’t have filters and people often use them for long periods, the health risks might be even greater. Hookahs are usually shared, so there’s the additional risk from germs being passed around along with the pipe.
Also beware of electronic cigarettes (e-cigarettes), which contain cancer-causing chemicals and other toxins, including a compound used in antifreeze. These battery-operated devices use cartridges filled with nicotine, flavorings, and other chemicals and convert them into a vapor that’s inhaled by the user.
For some time in the US, hookahs and e-cigarettes have not been regulated or studied by the U.S. Food and Drug Administration (FDA), so little has been known about their safety. But as of August 2016, new rules are in place to monitor these products. In the future, hookahs and e-cigarettes that are sold will need to be approved by the FDA, and companies will need to post health warnings so that people know their risks. But one thing is still certain: there’s no such thing as a “safe” nicotine product.
How Smoking Affects Your Health
There are no physical reasons to start smoking. The body doesn’t need tobacco the way it needs food, water, sleep, and exercise. And many of the chemicals in cigarettes, like nicotine and cyanide, are actually poisons that can kill in high enough doses.
The body is smart. It goes on the defense when it’s being poisoned. First-time smokers often feel pain or burning in the throat and lungs, and some people feel sick or even throw up the first few times they try tobacco.
The consequences of this poisoning happen gradually. Over the long term, smoking leads people to develop health problems like heart disease, stroke, emphysema (breakdown of lung tissue), and many types of cancer — including lung, throat, stomach, and bladder cancer. People who smoke can develop skin problems like psoriasis (a type of rash), and are more likely to get wrinkles. Also, they have an increased risk of infections like bronchitis and pneumonia.
Many of these diseases limit a person’s ability to be normally active, and they can be fatal. In the United States, smoking is responsible for about 1 out of 5 deaths.
Smokers not only develop wrinkles and yellow teeth, they also lose bone density, which increases their risk of osteoporosis, a condition that causes older people to become bent over and their bones to break more easily. Smokers also tend to be less active than nonsmokers because smoking affects lung power.
Smoking can also cause fertility problems and can impact sexual health in both men and women. Girls who are on the Pill or other hormone-based methods of birth control (like the patch or the ring) increase their risk of serious health problems, such as heart attacks, if they smoke.
The consequences of smoking may seem very far off, but long-term health problems aren’t the only hazard of smoking. Nicotine and the other toxins in cigarettes, cigars, and pipes can affect a person’s body quickly, which means that teen smokers have many of these problems:
- Bad breath. Cigarettes leave smokers with a condition called halitosis, or persistent bad breath.
- Bad-smelling clothes and hair. The smell of stale smoke tends to linger — not just on people’s clothing, but on their hair, furniture, and cars. And it’s often hard to get the smell of smoke out.
- Reduced athletic performance. People who smoke usually can’t compete with nonsmoking peers because the physical effects of smoking (like rapid heartbeat, decreased circulation, and shortness of breath) harm sports performance.
- Greater risk of injury and slower healing time. Smoking affects the body’s ability to produce collagen, so common sports injuries, such as damage to tendons and ligaments, will heal more slowly in smokers than nonsmokers.
- Increased risk of illness. Studies show that smokers get more colds, flu, bronchitis, and pneumonia than nonsmokers. And people with certain health conditions, like asthma, become more sick if they smoke (and often if they’re just around people who smoke). Because teens who smoke as a way to manage weight often light up instead of eating, their bodies also lack the nutrients they need to grow, develop, and fight off illness properly.
Kicking Butts and Staying Smoke-Free
All forms of tobacco — cigarettes, pipes, cigars, hookahs, and smokeless tobacco — are health hazards. It doesn’t help to substitute products that seem like they’re better for you than regular cigarettes, such as e-cigarettes or filtered or low-tar cigarettes.
The only thing that really helps a person avoid the problems associated with smoking is staying smoke-free. This isn’t always easy, especially if everyone around you is smoking and offering you cigarettes. It may help to have your reasons for not smoking ready for times you may feel the pressure, such as “I just don’t like it” or “I want to stay in shape for soccer” (or football, basketball, or other sport).
The good news for people who don’t smoke or who want to quit is that studies show that the number of teens who smoke has dropped dramatically. Today, about 10% of high school students smoke — which means 9 out of 10 don’t.
If you do smoke and want to quit, you have lots of information and support available. Different approaches to quitting work for different people. For some, quitting cold turkey is best. Others find that a slower approach is the way to go. Some people find that it helps to go to a support group especially for teens. These are sometimes sponsored by local hospitals or organizations like the American Cancer Society. The Internet offers a number of good resources to help people quit smoking.
When quitting, it can be helpful to realize that the first few days are the hardest. So don’t give up. Some people find they have a few relapses before they manage to quit for good.
Staying smoke-free will give you a whole lot more of everything — more energy, better performance, better looks, more money in your pocket, and in the long run, more life to live!

Hand, foot, and mouth disease (HFMD) is a common infection caused by a group of viruses.[10] It typically begins with a fever and feeling generally unwell.[10] This is followed a day or two later by flat discolored spots or bumps that may blister, on the hands, feet, and mouth, and occasionally buttocks and groin.[1][2][11] Signs and symptoms normally appear 3–6 days after exposure to the virus.[4] The rash generally resolves on its own in about a week.[5] Fingernail and toenail loss may occur a few weeks later, but they will regrow with time.[3]
The viruses that cause HFMD are spread through close personal contact, through the air from coughing, and the feces of an infected person.[8] Contaminated objects can also spread the disease.[8] Coxsackievirus A16 is the most common cause and Enterovirus 71 is the second-most common cause.[6] Other strains of coxsackievirus and enterovirus can also be responsible.[6][12] Some people may carry and pass on the virus despite having no symptoms of disease.[10] Other animals are not involved.[8] Diagnosis can often be made based on symptoms.[7] Occasionally a throat or stool sample may be tested for the virus.[7]
Handwashing may prevent spread and those infected should not go to work, daycare, or school.[8] No antiviral medication or vaccine is available, but development efforts are underway.[13] Most cases require no specific treatment.[5] Simple pain medication such as ibuprofen or numbing mouth gel may be used.[9] Occasionally intravenous fluids are given to children who are unable to drink enough.[9] Rarely viral meningitis or encephalitis may complicate the disease.[3]
HFMD occurs in all areas of the world.[14] It often occurs in small outbreaks in nursery schools or kindergartens.[1] Large outbreaks have been occurring in Asia since 1997.[14] It usually occurs during the spring, summer, and fall months.[14] Typically it occurs in children less than five years old, but can occasionally occur in adults.[1][10] HFMD should not be confused with foot-and-mouth disease (also known as hoof-and-mouth disease) which mostly affects livestock.[15]
Signs and symptoms
Common constitutional signs and symptoms of the HFMD include fever, nausea, vomiting, feeling tired, generalized discomfort, loss of appetite, and irritability in infants and toddlers. Skin lesions frequently develop in the form of a rash of flat discolored spots and bumps which may be followed by vesicular sores with blisters on palms of the hands, soles of the feet, buttocks, and sometimes on the lips.[16] The rash is rarely itchy for children,[4] but can be extremely itchy for adults. Painful facial ulcers, blisters, or lesions may also develop in or around the nose or mouth.[1][17][18] HFMD usually resolves on its own after 7–10 days.[17] Most cases of the disease are relatively harmless, but complications including encephalitis, meningitis, and paralysis that mimics the neurological symptoms of polio can occur.[19]
Cause
The viruses that cause the disease are of the Picornaviridae family. Coxsackievirus A16 is the most common cause of HFMD.[6] Enterovirus 71 (EV-71) is the second-most common cause.[6] Many other strains of coxsackievirus and enterovirus can also be responsible.[6][12]
Transmission
HFMD is highly contagious and is transmitted by nasopharyngeal secretions such as saliva or nasal mucus, by direct contact, or by fecal-oral transmission.
Child care settings are the most common places for HMFD to be contracted because of the bathroom training, diaper changes, and that children often put their hands into their mouths.[18] Children who do not attend a preschool or kindergarten were found to be more susceptible to the disease.[20] HFMD is contracted through nose and throat secretions such as saliva, sputum, nasal mucus and as well as fluid in blisters, and stool.[20]
Diagnosis
A diagnosis usually can be made by the presenting signs and symptoms alone.[17] If the diagnosis is unclear, a throat swab or stool specimen may be taken to identify the virus by culture.[17] The common incubation period (the time between infection and onset of symptoms) ranges from three to six days.[4] Early detection of HFMD is important in preventing an outbreak in the pediatric population.[21]
Prevention
Preventive measures include avoiding direct contact with infected individuals (including keeping infected children home from school), proper cleaning of shared utensils, disinfecting contaminated surfaces, and proper hand hygiene. These measures have been shown to be effective in decreasing the transmission of the viruses responsible for HFMD.[17][22]
Protective habits include hand washing and disinfecting surfaces in play areas.[20] Breast-feeding has also shown to decrease rates of severe HFMD, though does not reduce the risk for the infection of the disease.[20]
Vaccine
A vaccine known as the EV71 vaccine is available to prevent HFMD in China as of December 2015.[23] No vaccine is currently available in the United States.[22]
Treatment
Medications are usually not needed as hand, foot, and mouth disease is a viral disease that typically resolves on its own. Currently, there is no specific curative treatment for hand, foot and mouth disease.[17] Disease management typically focuses on achieving symptomatic relief. Pain from the sores may be eased with the use of analgesic medications. Infection in older children, adolescents, and adults is typically mild and lasts approximately 1 week, but may occasionally run a longer course. Fever reducers and lukewarm baths can help decrease body temperature.
A minority of individuals with hand, foot and mouth disease may require hospital admission due to complications such as inflammation of the brain, inflammation of the meninges, or acute flaccid paralysis.[12] Non-neurologic complications such as inflammation of the heart, fluid in the lungs, or bleeding into the lungs may also occur.[12]
Complications
Complications from the viral infections that cause HFMD are rare, but require immediate medical treatment if present. HFMD infections caused by Enterovirus 71 tend to be more severe and are more likely to have neurologic or cardiac complications including death than infections caused by Coxsackievirus A16.[17] Viral or aseptic meningitis can occur with HFMD in rare cases and is characterized by fever, headache, stiff neck, or back pain.[12][17] The condition is usually mild and clears without treatment; however, hospitalization for a short time may be needed. Other serious complications of HFMD include encephalitis (swelling of the brain), or flaccid paralysis in rare circumstances.[16][17]
Fingernail and toenail loss have been reported in children 4–8 weeks after having HFMD.[4] The relationship between HFMD and the reported nail loss is unclear; however, it is temporary and nail growth resumes without treatment.[4][24]
Minor complications due to symptoms can occur such as dehydration, due to mouth sores causing discomfort with intake of foods and fluid.[25]
Epidemiology
Hand, foot and mouth disease most commonly occurs in children under the age of 10.[4][17] It tends to occur in outbreaks during the spring, summer, and autumn seasons.[6] This is believed to be due to heat and humidity improving spread.[20] HFMD is more common in rural areas than urban areas; however, socioeconomic status and hygiene levels need to considered.[26] Poor hygiene is a risk factor for HFMD.[27]
Outbreaks have occurred in China, Japan, Hong Kong, the Republic of Korea, Malaysia, Singapore, Thailand, Taiwan, and Vietnam.[20] HFMD most commonly affects young children under the age of 10 and more often under the age of 5, but can also affect adults with varying symptoms.[18]
Since 1997 there have been 71 large enterovirus outbreaks reported, mostly in East and South East Asia, primarily affecting children.[20] From the years 2008 to 2014, more than 1 million HFMD cases have been reported in China each year.[28]
Outbreaks
- In 1998, there was an outbreak in Taiwan, affecting mainly children.[29] There were 405 severe complications, and 78 children died.[30] The total number of cases in that epidemic is estimated to have been 1.5 million.[6]
- In 2008 an outbreak in China, beginning in March in Fuyang, Anhui, led to 25,000 infections, and 42 deaths, by May 13.[6] Similar outbreaks were reported in Singapore (more than 2,600 cases as of April 20, 2008),[31] Vietnam (2,300 cases, 11 deaths),[32] Mongolia (1,600 cases),[33] and Brunei (1053 cases from June–August 2008)[34]
- In 2009 17 children died in an outbreak during March and April 2009 in China’s eastern Shandong Province, and 18 children died in the neighboring Henan Province.[35] Out of 115,000 reported cases in China from January to April, 773 were severe and 50 were fatal.[36]
- In 2010 in China, an outbreak occurred in southern China’s Guangxi Autonomous Region as well as Guangdong, Henan, Hebei and Shandong provinces. Until March 70,756 children were infected and 40 died from the disease. By June, the peak season for the disease, 537 had died.[37]
- The World Health Organization reporting between January to October 2011 (1,340,259) states the number of cases in China had dropped by approx 300,000 from 2010 (1,654,866) cases, with new cases peaking in June. There were 437 deaths, down from 2010 (537 deaths).[38]
- In December 2011, the California Department of Public Health identified a strong form of the virus, coxsackievirus A6 (CVA6), where nail loss in children is common.[39]
- In 2012 in Alabama, United States there was an outbreak of an unusual type of the disease. It occurred in a season when it is not usually seen and affected teenagers and older adults. There were some hospitalizations due to the disease but no reported deaths.[40]
- In 2012 in Cambodia, 52 of 59 reviewed cases of children reportedly[41] dead (as of July 9, 2012) due to a mysterious disease were diagnosed to be caused by a virulent form of HFMD.[42] Although a significant degree of uncertainty exists with reference to the diagnosis, the WHO report states, “Based on the latest laboratory results, a significant proportion of the samples tested positive for enterovirus 71 (EV-71), which causes hand foot and mouth disease (HFMD). The EV-71 virus has been known to generally cause severe complications amongst some patients.”[43]
- HFMD infected 1,520,274 people with up to 431 deaths reported at the end of July in 2012 in China.[44]
Jika tidak minum air manis setiap hari, tiada gula dalam badan?
Fakta atau mitos :
“Sekiranya saya tidak minum air manis setiap hari, saya tidak ada gula dalam badan” ?
 Gambar 1 : Minuman manis (sumber : freepik.com)
Gambar 1 : Minuman manis (sumber : freepik.com)
Pernyataan bahawa “penghidap diabetes memerlukan air manis setiap hari” adalah tidak benar. Karbohidrat kompleks seperti buah-buahan dan makanan bijirin (nasi, mee dan roti) juga membekalkan tenaga atau kalori. Pengambilan gula yang tinggi boleh menyebabkan peningkatan glukosa dalam darah yang tidak terkawal dan menyebabkan pertambahan berat badan.
Makanan berkarbohidrat membekalkan gula dan boleh digunakan oleh badan untuk menghasilkan tenaga, disimpan di dalam hati dan otot sebagai glikogen atau ditukarkan kepada lemak sekiranya tidak digunakan.
Sel badan dan sistem saraf bergantung kepada glukosa. Tanpa gula, badan akan memaksa tisu protein untuk dipecahkan kepada glukosa dan memetabolismakan tenaga untuk menghasilkan keton daripada lemak.
Kehadiran insulin (hormon pankreas) berfungsi untuk mengangkut gula dalam darah ke sel-sel badan. Sekiranya insulin dalam badan berkurangan atau tiada terutama bagi penghidap diabetes, gula dalam darah akan meningkat.
Gula ringkas mengandungi kalori tetapi kurang mengandungi vitamin, mineral dan serat (fibre). Karbohidrat ringkas boleh terdapat dalam makanan seperti :
- Gula pasir
- Gula-gula
- Minuman berkarbonat seperti soda
- Minuman sirap atau kordial
 Gambar 2 : Contoh makanan & minuman karbohidrat ringkas (sumber : fitnessgoals.com)
Gambar 2 : Contoh makanan & minuman karbohidrat ringkas (sumber : fitnessgoals.com)
Keperluan karbohidrat adalah antara 40 hingga 60% daripada saranan kalori sehari. Karbohidrat kompleks adalah makanan yang hadir dalam makanan mengandungi serat, vitamin dan mineral dan membekalkan tenaga yang utama.
Untuk meningkatkan pengambilan karbohidrat kompleks dan mendapat zat yang sihat , amalkan perkara seperti :
- Makan lebih sayur-sayuran dan buah-buahan
- Makan lebih nasi bijirin penuh, roti dan bijirin
- Makan lebih legum. (Contoh: kacang tanah, kacang pea, lentil)
 Gambar 3 : Sayur, buah dan karbohidrat (sumber : ectomorphworkout.org)
Gambar 3 : Sayur, buah dan karbohidrat (sumber : ectomorphworkout.org)
Saranan pengambilan makanan tinggi karbohidrat mengikut saiz hidangan :
| Sayur-sayuran | 1 cawan sayur-sayuran mentah, atau |
| ½ cawan sayur-sayuran yang dimasak | |
| Buah-buahan | 1 biji sederhana buah-buahan berbiji (contoh: epal, oren, lai), |
| 1 potong buah-buahan (contoh : betik, tembikai, nenas) | |
| Roti dan bijirin | 1 potong roti, atau |
| ½ cawan nasi/ pasta/mee, atau | |
| ½ cawan kekacang | |
| Produk tenusu | 1 cawan susu skim, atau |
| susu rendah lemak |
{Link: Karbohidrat Kompleks}
Penghadaman dan penyerapan karbohidrat
Gula dan makanan berkarbohidrat akan dihadam kepada molekul yang kecil iaitu glukosa dan diserap ke dalam badan untuk digunakan.
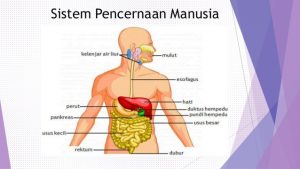 Gambar 4 : Sistem pencernaan manusia (sumber : https://image.slidesharecdn.com)
Gambar 4 : Sistem pencernaan manusia (sumber : https://image.slidesharecdn.com)
Di dalam mulut :
Makanan berkarbohidrat akan dipecahkan kepada polisakarida dan maltosa dengan bantuan enzim amilase. Kenyataannya, jika anda makan makanan berkanji seperti biskut, anda akan dapat merasa manis dengan bantuan enzim amilase kerana makanan berada di dalam mulut hanya sementara. Penghadaman karbohidrat berlaku hanya sementara di dalam mulut dan terus masuk ke dalam salur penghadaman.
Di perut :
Makanan yang ditelan akan menjadi bolus bercampur dengan asid di dalam perut dan enzim penghadam protein. Enzim akan memecahkan makanan berkanji. Manakala, makanan yang mengandungi serat akan melambatkan pengosongan makanan di perut. Ini menyebabkan perut akan merasa penuh dan kenyang berpanjangan.
Di usus kecil :
Makanan berkarbohidrat paling banyak diserap di sini. Enzim penghadam karbohidrat iaitu amilase pankreatik memasuki usus kecil melalui salur pankreas. Karbohidrat dalam bentuk polisakarida akan dipecahkan kepada molekul yang lebih kecil seperti di bawah :
- Maltosa : Glukosa + Glukosa
- Sukrosa : Glukosa + Fruktosa
- Laktosa : Glukosa + Galaktosa
Di peringkat ini semua makanan yang berkarbohidrat telah dipecahkan kepada molekul yang lebih kecil. Kebanyakan adalah dalam bentuk glukosa.
Di usus besar :
Dalam masa 1 hingga 4 jam selepas makan, semua gula dan makanan yang berkanji telah dihadamkan, kecuali serat akan tinggal di salur penghadaman. Serat akan menarik air, seterusnya akan melembutkan najis di usus besar. Di sini juga, terdapat bakteria yang memfermentasi serat menghasilkan air, gas dan lemak berantai pendek. Usus menggunakan molekul lemak ini untuk tenaga.
Oleh itu, serat juga boleh menyumbangkan tenaga bergantung kepada berapa banyak yang dipecahkan oleh bakteria dan asid lemak yang diserap.
Glukosa boleh dihadam di dalam mulut dan yang paling penting akan diserap di usus kecil. Glukosa dan galaktosa akan diangkut melalui usus kecil ke sel-sel badan. Manakala, fruktosa akan diserap secara facilitated diffusion, di mana akan melambatkan kenaikan gula dalam darah.
Karbohidrat yang tidak berantai (monosakarida) akan dihadam dengan perlahan dan akan meningkatkan gula dalam darah dengan sedikit. Darah akan mengalir dari usus ke hati, sel-sel di sini akan mengambil fruktosa dan galaktosa dan akan ditukarkan kepada glukosa. Seterusnya meningkatkan glukosa dalam darah.
Kesimpulan
Pengambilan makanan berkarbohidrat boleh menyumbang kepada penghasilan gula dalam badan dan berfungsi untuk menghasilkan tenaga dalam tubuh badan.
Oleh itu, penghidap diabetes tidak perlu mengambil gula setiap hari kerana gula sentiasa ada dalam badan iaitu daripada pengambilan makanan berkarbohidrat.
Rujukan :
- Medline Plus (2012) Carbohydrates. Retrieved: September 21, 2012. http://www.nlm.nih.gov/medlineplus/ency/article/002469.htm
- Sharon R. R., Kathyryn P. & Ellie W. (2006) The carbohydrate: Sugars, Starches and Fibers. Understanding normal and clinical nutrition. 7th edition. Publisher: Thompson Higher Education 10 Davis Drive Belmont, CA 94002-3098 USA.
- Wikipedia (2008) Carbohydrate. Retrieved: September 21, 2012. Wiki: http://en.wikipedia.org/wiki/Carbohydrate
Sumber : pendidikanpesakit.myhealth.gov.my




